 Pennsylvania Auditor General Timothy L. DeFoor today [Aug. 28] released a performance audit that showed Pennsylvania taxpayers paid $7 million more for Medicaid prescription drug benefits than they should have during 2022 because of lack of oversight by the Department of Human Services and spread pricing by pharmacy benefit managers (PBMs).
Pennsylvania Auditor General Timothy L. DeFoor today [Aug. 28] released a performance audit that showed Pennsylvania taxpayers paid $7 million more for Medicaid prescription drug benefits than they should have during 2022 because of lack of oversight by the Department of Human Services and spread pricing by pharmacy benefit managers (PBMs).
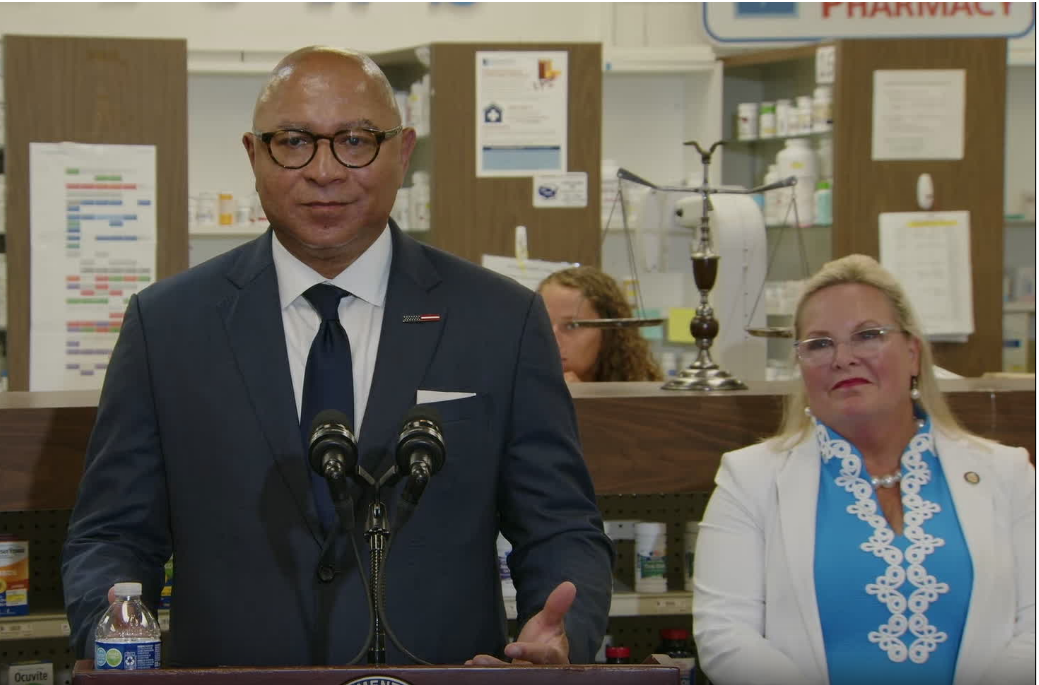
“Our auditors found evidence of spread pricing, inadequate monitoring by DHS and overcharging of taxpayers by PBMs, resulting in a loss of $7 million in taxpayer money in just 2022 alone,” Auditor General DeFoor said. “PBMs are counting on the fact that no one is checking their reporting so they can get paid a higher rate and still collect a fee from the pharmacy. We made recommendations to ensure more accountability and process improvements, but what really needs to happen here are changes in the law.”
DHS contracts with managed care organizations (MCOs) to implement the Physical HealthChoices Medicaid program. MCOs then contract with PBMs to manage the prescription drug benefits for the program. According to DHS, more than 2.8 million Pennsylvanians utilize this taxpayer-funded benefit.
Spread pricing happens when a PBM charges an insurance plan more for a prescription drug than what is paid to the pharmacy for that medication. The PBM keeps the fee as another revenue source.
“This is not just a process issue,” Auditor General DeFoor added. “Pharmacies are going out of business because of the impact of spread pricing. Spread pricing in any form is hurting the very people we promised to help.”
The auditors found that DHS failed to effectively monitor the HealthChoices program’s pharmacy expenditures of $4.6 billion in 2022. This resulted in undisclosed spread pricing in which PBMs were not reporting transmission fees charged to pharmacies to the MCOs and DHS. This lack of transparency resulted in overstated pharmacy data.
In addition, auditors found that DHS did not effectively monitor contracts between MCOs and PBMs. DHS did not have written policies and procedures for its contract monitoring efforts and did not verify that PBM contracts complied with the HealthChoices contract.
Regarding the PBM PerformRX, auditors found that while the company was transparent with pharmacies regarding the additional fees, it never provided that information to the MCOs or DHS. PerformRX is legally required to inform the MCO and DHS of any fees it charges to pharmacies.
“A lot of work has been done on both sides of the aisle to implement changes to how PBMs operate in Pennsylvania,” Auditor General DeFoor said. “Now is the time to focus on the taxpayer-funded Medicaid system and close the loophole that allows PBMs to charge pharmacies transmission fees. We need changes in the law to make sure there is no room for spread pricing to occur with our tax dollars and the law needs to clearly define that DHS is accountable for the information reported to them by their contractors.”
The audit objectives were to:
• Determine whether DHS effectively monitored the PBMs’ pharmacy claims, including, but not limited to, the accuracy of the pharmacy information used to prepare the capitation rates for the HealthChoices Medicaid program.
• Determine whether DHS effectively monitored the PBMs’ contracts to ensure compliance and transparency for the HealthChoices Medicaid program; and
• Determine if the PBM PerformRX was compliant with 62 P.S. § 449(h)(3) and (4) of the Human Services Code (as amended by Act 120 of 2020) regarding charges and fees paid to the PBM by the pharmacies, or pharmacy service organizations, as compared to the corresponding amounts billed to the applicable HealthChoices MCOs to ensure transparency, compliance, and accountability for the HealthChoices Medicaid Program.
To view and find more information on the audit, visit the Be Audit Smart page on www.paauditor.gov.
The above article courtesy of Pennsylvania Pharmacists Association.
